Plasma helps save the life of a pregnant mother diagnosed with CIDP
When Stephanie Patterson was pregnant with her second child in September 2020, she began to feel a tingling in her feet that wouldn’t go away. Her primary care physician ordered an electromyography (EMG) test, which evaluates nerve and muscle function. The results came back abnormal. Patterson was told she most likely had Charcot Marie Tooth (CMT) disease, which is a group of inherited disorders that cause nerve damage. Patterson was referred to a neurologist who told her that her symptoms were pregnancy-related and there wasn’t much that could be done for her until after she gave birth. At the time, Patterson was only ten weeks pregnant.
From there, Patterson’s symptoms quickly began to get worse. The tingling sensation moved up her legs and into her hips, and she began experiencing numbness in her hands, feet, and knees.
“I couldn’t lift myself off of the toilet,” says Patterson. “My husband had to help me in and out of bed. I fell a few times and needed assistance getting up. I remember thinking there is no way this is pregnancy related.”
After reaching back out to the neurologist, she was once again dismissed and told that these were merely side effects of her pregnancy. So, Patterson sought out a second opinion from a highly recommended neurologist who, after hearing her symptoms, told her to go to the emergency room immediately.
“It was in the ER that I finally got the attention I needed. I spent five days in the hospital, where I was properly diagnosed with chronic inflammatory demyelinating polyneuropathy (CIDP).”
CIDP is a rare disorder of the peripheral nerves that is characterized by progressive weakness and sensory loss. Immunoglobulin (Ig) replacement therapy, either intravenous (IVIG) or subcutaneous (SCIG), is one of the only U.S. Food and Drug Administration (FDA)-approved drugs for treating CIDP.
Ig refers to the liquid plasma component of blood that contains immunoglobulins or antibodies. Ig replacement therapies can only be manufactured with donated plasma. There is no synthetic option available because the complex mix of antibodies present in plasma cannot be recreated in a lab.
Patterson received her first dose of IVIG in the hospital after her diagnosis. She then received IVIG at home every three weeks and continues to receive IVIG treatments every four weeks for two days. Her full-time remote job gives her the flexibility for various doctor appointments and her monthly IVIG treatments. Patterson says that with these treatments, she’s seen a great improvement in her symptoms.
“Without plasma, I would not have a quality life. I would be wheelchair-bound and require full-time assistance for basic tasks. Plasma treatments give me my life and refresh my mobility every month. It allows me to walk and work, play with my kids, explore the world, and experience all the amazing joys in this life.”
Patterson believes in sharing her story wherever she can in order to raise awareness for chronic conditions and plasma donation, saying, “Most days, I look perfectly healthy on the outside. I may walk a little slower or need a cane, but no one would ever suspect that I have a chronic condition. When it does come up in conversation, I stress the importance of plasma donation and how it allows me to maintain my mobility.”
In May 2023, when GBS|CIDP Foundation asked their community to tell them about a hero in their life, Patterson submitted her home health infusion nurse, Randy. Patterson considers Randy to be part of her family, as he was her infusion nurse from the very beginning of her treatments.
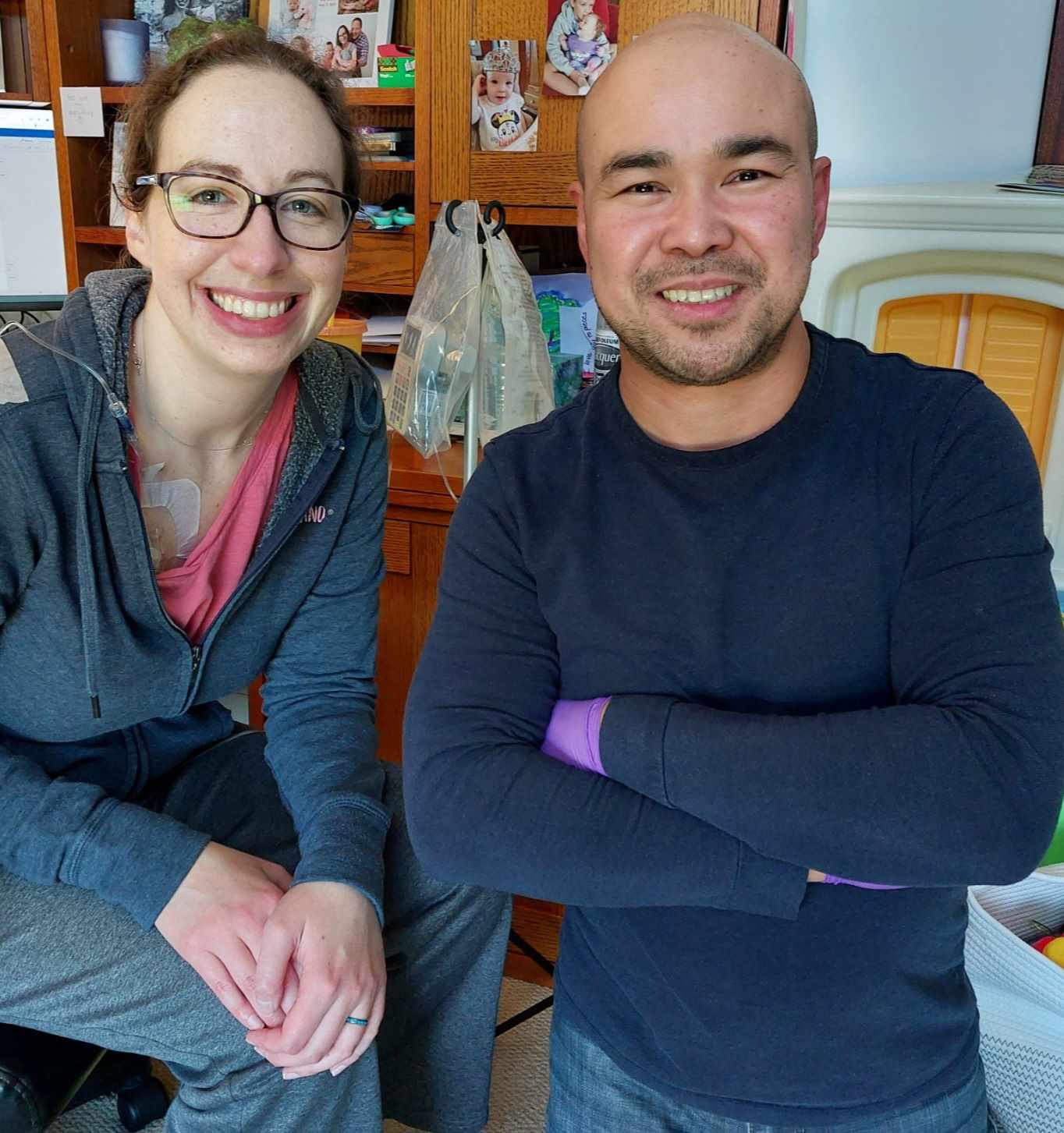
“I was very nervous to start treatments and had no idea what to expect, but he put my fears at ease. He ensures that I feel very comfortable during my treatments and advocates for me if I need supplies or additional care. My kids always ask when Nurse Randy will be coming over; he truly has become part of the family. I am grateful he's on this journey with me.”
Patterson, who lives in Pennsylvania with her husband and two children, says thanks to plasma donors, she’s been given the gift of life and mobility, allowing her to spend time with her family outside, whether it’s taking walks, visiting playgrounds, or having picnics. And while she says she knew a few individuals who donated plasma, she never realized the impact of plasma donation until after her CIDP diagnosis.
“I can’t say thank you enough. I hope you know how important you are to me and my family. Everyone who plays a part in the process of making IVIG has a direct impact on providing me with the gift of a more normal life,” says Patterson. “I hope my story inspires more people to learn more about the process and consider giving the gift of mobility to individuals like myself.”
Learn more about plasma donation and how you can make a difference in lives like Patterson’s and others living with CIDP.
More Heroes

Find a donation center
Donate blood plasma. Be a hero. Locate a plasma donation center near you.

